Rheumatology is a specialty dedicated to the study of rheumatic diseases and musculoskeletal disorders, which account for approximately 10% of primary care office visits. The diagnostic approach usually includes a complete medical history, physical examination with the use of classification criteria and, if indicated, laboratory tests and imaging studies.
Patients with rheumatic conditions present to physicians with a myriad of different complaints. Although signs and symptoms can be localized and specific for a certain diagnosis, on many occasions symptoms are ill-defined and physical diagnosis is subtle.
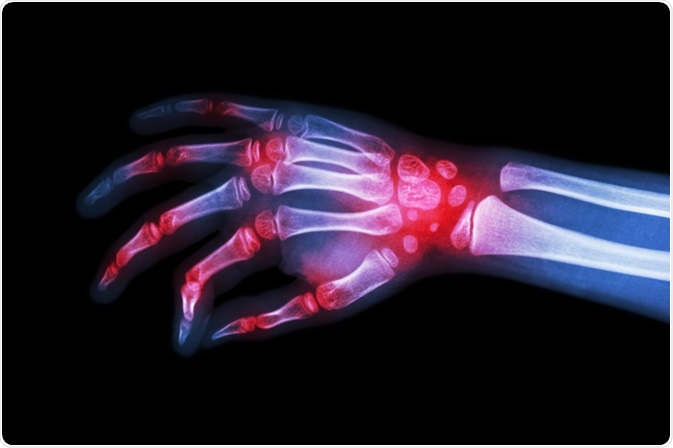
Image Credit: Puwadol Jaturawutthichai / Shutterstock
Physical examination
Rheumatic illnesses lend themselves well to a systematic approach of diagnosis based on demographics and pattern of muscle, joint and organ involvement. For example, a young woman with diffuse articular pain and malar rash should be suspicious of systemic lupus erythematosus, whereas a painful first metacarpal joint of acute onset should evoke the diagnosis of gout.
When an individual presents with a musculoskeletal complaint, pain is usually the driving force. The important aspect of physical examination is to determine the symmetry of joint involvement, the number and location of joints affected, as well as the presence of inflammation.
The mode of onset and evolution of symptoms over time is very helpful in establishing a correct diagnosis. For the majority of chronic arthropathies such as rheumatoid arthritis, the onset is typically subacute, occurring over weeks to months rather than hours to days. On the other hand, attacks of gout and septic arthritis present acutely, reaching a peak within hours.
Diagnostic and classification criteria
As most rheumatic diseases are syndromic without definite diagnostic features, it is pivotal to establish criteria that ensure uniformity of diagnosis, classification and epidemiological studies. Disease-specific criteria that contributed substantially to the practice and progress of rheumatology have been developed for the majority of rheumatic disorders.
In short, classification criteria aim to distinguish patients with the disease in question from those without the disease. Some experts advocate the use of diagnostic criteria as a valuable screening tool for primary care, especially when striving to identify patients in the early stages of rheumatic conditions.
Criteria have been also developed to assess disease activity, such as DAS-28 for rheumatoid arthritis or SLEDAI for systemic lupus erythematosus. They are helpful not only in research settings but also in daily clinical practice, as treatments can be tailored to achieve maximum disease control in an objective way.
Laboratory testing and imaging studies
When they are carefully used, laboratory tests can be very specific and help considerably in establishing a correct diagnosis. A basis of early screening is to determine erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), which are both parts of the acute phase response.
Antinuclear antibodies (ANA) are present in a wide array of autoimmune and connective tissue diseases. While nearly all patients with systemic lupus are ANA-positive, the high number of false positives cases hampers its utility as a screening test. Rheumatoid factor (RF) is commonly used in the diagnosis of rheumatoid arthritis, but its sensitivity varies depending on the patient population.
New tests, such as the cyclic citrullinated protein antibody, are introduced to improve the early identification of patients with rheumatoid arthritis – namely those with a prognosis for a more aggressive disease. Furthermore, antikeratin, anti-RA33, anti-p68 and anti-Sa autoantibodies have been shown to have more than 90% specificity for this disease.
Further Reading
 Factors associated with diagnostic delay in Familial Mediterranean Fever
Factors associated with diagnostic delay in Familial Mediterranean Fever